A novel treatment for pulmonary fibrosis may be located within the lungs themselves. The same alveolar epithelial cells (AECs) that can become fibrotic can also become reparative, at least in mouse models. It is not clear how to harness that plasticity therapeutically, but the potential exists, said Zea Borok, MD, ATSF, the Helen M. Ranney professor of medicine and chair of the Department of Medicine at the University of California, San Diego.
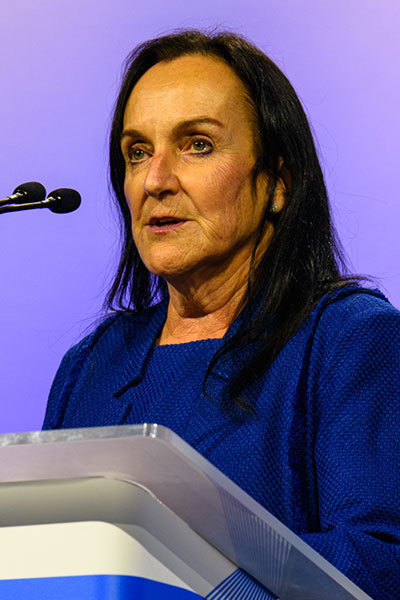
Dr. Borok delivered the J. Burns Amberson Lecture, “Type I, Type II, and Everything in Between: Unlocking the Plasticity of Alveolar Epithelial Cells” during Sunday’s Awards Ceremony. The alveolar epithelium is composed of two cell types, Type II (AT2) and Type I (AT1), she explained. AT2 cells are cuboidal, surfactant-producing cells with lamellar bodies. AT1 cells are large, squamous cells with attenuated cytoplasmic processes that provide the major surface for gas exchange.
It has long been known that AT2 cells can serve as progenitors for AT1 cells following lung injury, but AT1 cells were thought to be terminally differentiated.
“The reality is more complex, as recent single-cell data show,” she said. “AT1 cells retain plasticity and seem to act as either reparative or pathogenic.”
Why study the alveolar epithelium?
“It was not an intuitive subject,” said Dr. Borok, whose work began in the 1980s. “It was a major area of focus of the lab I was joining. And very few people were studying it at the time. The alveolar epithelium was an opportunity.”
Dr. Borok and her colleagues soon noticed that AECs gradually differentiate in vitro. AT2 cells take on morphologic features of AT1 cells and express AT1 cell phenotypic markers.
The observation was met with skepticism, she said, but was subsequently corroborated by multiple labs using disparate systems. It raised questions about AEC plasticity and whether AT1 cells can transform into AT2 cells.
AT1 cells treated with keratinocyte growth factor showed changes in cell markers suggesting that plasticity might work in both directions. Other labs soon found that AT1 cells can give rise to cells that express AT2 and other cell-type markers.
Genome-wide gene expression and chromatin immunoprecipitation sequencing data found that AEC differentiation is regulated by networks of transcription factors acting in concert. Both AT2 and AT1 cells enter an intermediate transitional phase characterized by the expression of keratin-8 protein that can be induced by lung injury.
These transitional cells are enriched for markers of senescence and markers consistent with epithelial-mesenchymal transition. The persistence of these transitional cell states is associated with fibrosis. These upregulated mesenchymal markers are also seen in idiopathic pulmonary fibrosis, suggesting that reprogrammed AECs may create a profibrotic environment.
“If AECs get stuck in transition, they become pathogenic,” Dr. Borok said. “This was a real paradigm shift away from inflammation to a central role for alveolar epithelium in pulmonary fibrosis.”
But transition need not lead to pathogenesis. Work with Claudin 18 knockout mice led to the surprising finding that CLDN18 KO lungs and stomachs are enlarged by about 30 percent. CLDN18 KO lungs have increased numbers of AT2 cells with increased proliferation. They are also protected from bleomycin injury, which kills 50 percent of wild-type mice.
CLDN18 KO lungs have increased KRT8+ cells without fibrosis. Single-cell RNA-seq revealed that CLDN18 KO mice had a shift toward transitional AT1 cells with accelerated differentiation of AT2 to AT1 cells. In this model, KRT8+ cells are reparative, not pathogenic.
“The jury is still out on this, and we still need to figure out if we can push them toward reparative, but we want to harness plasticity to promote regeneration,” Dr. Borok said.
Extend Your Learning Beyond San Francisco with ATS 2025 Conference Highlights

With so many valuable educational opportunities offered during the ATS 2025 International Conference, attendees are often forced to decide which sessions to prioritize. That’s why the Society is offering three ATS 2025 Conference Highlights packages for those unable to attend ATS 2025 San Francisco or attendees interested in continuing their education after the conference. Check out the packages and pick the one that’s right for you. Learn at your own pace, whenever and wherever you are!

