
Adult lung disease seldom begins de novo. Growing evidence points to early life as a key formative period for pulmonary disease in adulthood.
“Lung growth tracks the growth of the rest of the body,” said Erick Forno, MD, MPH, ATSF, director of the Pediatric Asthma Center and associate professor of pediatrics and clinical and translational science, University of Pittsburgh Medical Center Children’s Hospital Pittsburgh. “Any disruption, injury, or insult during early life, starting in utero, has an enormous impact on adult lung function.”
Dr. Forno was part of the ATS President’s Symposium: Early Life Determinants (Antecedents) of Adult Lung Disease. This session will be included in the On-Demand Highlights available through the ATS Store this summer.

Multiple studies confirm that adults with COPD and other lung diseases commonly had asthma or other lung disorders as young children. Conversely, premature birth and the associated lung damage confer up to a threefold risk for adult asthma and a 20-fold risk for adult COPD.
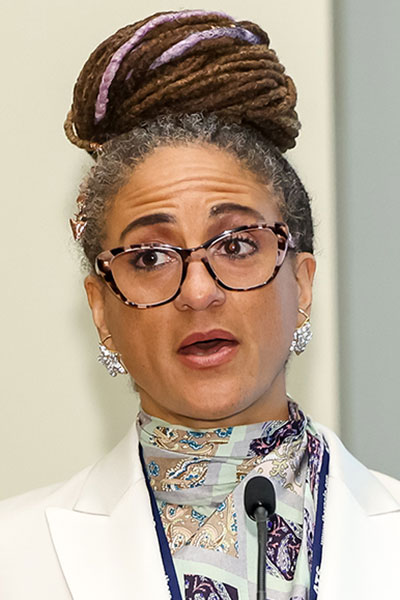
Lung health begins in childhood, and the children are not OK, said MeiLan K. Han, MD, MS, ATSF, professor and chief of pulmonary and critical care, University of Michigan School of Medicine. The most common cause of death in the U.S. in 2021 was refractory respiratory failure. But COVID-19 was not the most important player.
“The pandemic highlighted a crisis that was there before any of us were imperiled by the virus,” Dr. Han explained. “About half of adults with COPD enter adulthood with impaired lung function affected by childhood factors.”
Environmental exposures and nicotine exposure in utero can impact the lung health of children, she noted. Exposure to fine particulate matter and other airborne pollutants after birth can also exacerbate existing lung damage.

“Our lungs were in peril before COVID-19,” Dr. Han said. “It is our job as a community to make lung health a priority.”
One of the most neglected populations with pulmonary impairments includes people with sickle cell disease. SCD guidelines long ignored pulmonary function or advised against pulmonary function testing, yet acute chest syndrome, lower airway disease, sleep-disordered breathing and hypoxemia, and pulmonary vascular complications are common features of SCD.
“Pulmonary vascular complications in SCD start early,” said Benjamin T. Kopp, MD, MPH, ATSF, associate professor of pediatrics, co-director of the Center for CF and Airways Disease Research, and director of the Pulmonary Sickle Cell Program at Emory University School of Medicine. “Early is a good time to intervene.”
Some of those interventions are environmental. Studies have found that elevated levels of carbon monoxide and ozone are associated with fever in SCD; elevated particulate matter with ACS, pain, and other symptoms; and black carbon with pain and all other SCD symptoms.

As harmful as environmental and other insults can be to pulmonary function, the effects are exacerbated by preterm birth. Prematurity impairs the pulmonary and vascular systems, which can limit adult function. Children born severely premature have a stiffer, less recruitable pulmonary vascular bed by their first year, and most have mild to subclinical pulmonary hypertension, which increases over time.
“Premature birth is a ‘first hit’ for more severe pulmonary arterial hypertension in the vulnerable,” said Kara N. Goss, MD, associate professor of medicine and pediatrics, The University of Texas Southwestern Medical Center. “Preterm birth primes the pump for dysfunction.”
She advises providers to ask their patients with adult lung disease whether they were born prematurely because this is such a high-risk population.
So are children with interstitial lung disease. Pulmonary damage can be seen early in life, though the types of disease associated with ILD tend to differ in adults and children.

“There were concerted efforts to distinguish ILD in children from that in adults in the early 2000s,” said Lisa R. Young, MD, ATSF, chief of pulmonary and sleep medicine, professor of pediatrics, and the John M. Keating Endowed Chair in Pulmonary Medicine, Children’s Hospital of Philadelphia and Perelman School of Medicine at the University of Pennsylvania. “Today, we see ILD more as a continuum of disease.”
The formation of clinical and research networks in the U.S. and globally has fueled progress in childhood ILD, Dr. Young continued. One key result has been the discovery of the genetic basis for ILD and the growing role of genetic testing.
Gene identification and testing have spurred the development of multiple targeted agents, including patient-specific induced pluripotent stem cells. Early clinical trials of nintedanib showed acceptable safety and tolerability and favorable changes in forced expiry volume and arterial oxygen saturation.
Cystic fibrosis stands out as a success to be emulated in other pulmonary diseases.
“We have dramatically improved CF survival from dying in infancy to surviving at least into middle age,” said Jennifer L. Taylor-Cousar, MD, MSc, ATSF, president of the medical staff, medical director for clinical research services, co-director of the Adult Cystic Fibrosis Program, director of the Cystic Fibrosis Therapeutics Development Center Adult Program, and professor of internal medicine and pediatrics, National Jewish Health. “We now need clinicians who can treat adults with CF.”
That improvement began with the identification of the cystic fibrosis transmembrane conductance regulator gene responsible for CF. More than 2,500 variants have been identified with a wide variety of dysfunction, Dr. Taylor-Cousar said. CF inflammation begins in infancy, followed by declining lung function. The earlier treatment can begin, the more effective it can be.
Most people with CF are eligible for highly effective modulator therapy based on their genetic variant. Infants, if they have an eligible variant, can begin treatment after their first CF appointment.
Nucleic acid therapy is the current focus, Dr. Taylor-Cousar noted, and the first gene therapy trials are underway. Initial results could be reported later this year.
Extend Your Learning Beyond San Francisco with ATS 2025 Conference Highlights

With so many valuable educational opportunities offered during the ATS 2025 International Conference, attendees are often forced to decide which sessions to prioritize. That’s why the Society is offering three ATS 2025 Conference Highlights packages for those unable to attend ATS 2025 San Francisco or attendees interested in continuing their education after the conference. Check out the packages and pick the one that’s right for you. Learn at your own pace, whenever and wherever you are!

